The well-being of first responders has reached a critical tipping point. Chronic exposure to trauma, occupational stress, and unpredictable demands leaves many professionals in law enforcement, fire services, and emergency medicine vulnerable to burnout, depression, and disengagement. Traditional wellness assessments, while valuable for diagnostic clarity, fail to account for the broader dimensions of mental health or the dynamic needs of individuals working in high-stress environments.
The MyOmnia Wholeness Screener addresses this gap by offering a validated, science-driven solution grounded in prevention, adaptability, and user-centered design. Built specifically for high-risk populations, the Screener measures well-being across seven interconnected domains: Physical, Mental, Vocational and Financial, Social, Fun and Relaxation, Spiritual, and Purpose and Resilience. Using a tiered structure and adaptive logic, it activates subdomain items only when relevant, ensuring a brief yet highly personalized experience.
Uniquely, the Screener incorporates a Readiness Score to align support with motivation for change, and a Critical Item trigger to flag acute distress. These components support early identification, tailored care pathways, and real-time data insights for both individuals and organizations. Backed by a 2024 national validation study (Willoughby), the Screener has demonstrated high internal reliability and strong correlations with leading clinical measures such as CESD-R, STAI, and the BRS.
Unlike static assessments, MyOmnia offers AI-driven content recommendations, automated wellness tracking, and de-identified dashboards that help leadership teams make informed, preventive decisions. The platform moves organizations from crisis response to proactive well-being strategy.
MyOmnia is more than a tool, it is a comprehensive system for cultivating resilient, thriving individuals and workforces. In today’s climate of escalating stress and shrinking capacity for care, it offers a scalable, scientifically grounded, and mission-aligned path forward.

The mental health of first responders is an urgent and complex public health concern. Professionals in law enforcement, emergency medical services, fire services, and dispatch operate in environments characterized by unpredictability, trauma exposure, moral injury, and chronic occupational stress. These individuals face significantly higher risks of post-traumatic stress symptoms, depression, anxiety, and burnout compared to the general population (Carleton et al., 2018; Haugen, Evces, & Weiss, 2012). Despite these challenges, many mental health issues among first responders remain under-identified and under-treated, often due to stigma, limited access to specialized care, and the inadequacy of traditional wellness tools.
A key limitation of conventional mental health assessments is their reliance on static, symptom-focused models. Tools such as the Patient Health Questionnaire-9 (PHQ-9), developed by Kroenke, Spitzer, and Williams (2001), and the Generalized Anxiety Disorder-7 (GAD-7), developed by Spitzer, Kroenke, Williams, and Löwe (2006), while clinically validated and widely used, were designed primarily for diagnostic purposes in clinical settings. These tools measure the presence and severity of psychiatric symptoms but do not capture the broader dimensions of human functioning that influence long-term well-being, especially in high-risk professional groups.
These instruments also fail to assess critical factors such as readiness for change, the presence of protective factors like social support and purpose, or the complex interaction between domains such as physical health, emotional resilience, and vocational identity. This narrow scope limits their utility in proactive wellness programs, especially for first responders whose health challenges are often cumulative, interrelated, and deeply embedded in organizational and cultural contexts.
Recognizing this gap, MyOmnia has developed a novel solution: the MyOmnia Wholeness Screener. Rooted in prevention science and validated behavioral health frameworks, this tool redefines how mental wellness is assessed and supported in first responder populations. The Screener shifts the focus from diagnosing illness to measuring wholeness, a dynamic state of balance across multiple domains of life. Rather than treating well-being as the absence of symptoms, MyOmnia conceptualizes it as the presence of strength, resilience, purpose, and connection.
The MyOmnia Wholeness Screener is designed to meet the needs of both individuals and organizations. For users, it provides a brief yet comprehensive assessment experience that is adaptive, strength-based, and actionable. For employers and leadership teams, it offers aggregated insights into workforce well-being, enabling early intervention and informed resource allocation. Its integration of core wellness domains, readiness indicators, and AI-driven follow-up content makes it a highly responsive tool for addressing the evolving mental health needs of first responders.
This white paper presents the scientific rationale, structure, scoring system, and validation outcomes of the MyOmnia Wholeness Screener. It also compares this model to traditional assessment tools and explores its practical applications in both individual care and organizational strategy.
Understanding the concept of "wholeness" is central to appreciating the design, intent, and clinical utility of the MyOmnia Wholeness Screener. This section provides a concise summary of how the term is defined within the MyOmnia model and why it forms the foundation for a more comprehensive, individualized, and preventive approach to mental wellness, particularly for first responders and high-stress professionals.
In contrast to traditional models that measure well-being through isolated metrics such as stress levels or depressive symptoms, wholeness is conceptualized as a multidimensional and dynamic state of health. It reflects an individual's functioning across several life domains, encompassing not just physical and emotional health but also purpose, relationships, spirituality, and the capacity to engage meaningfully with life.
This integrated perspective is especially important in professions where stressors are chronic, systemic, and often unspoken. First responders regularly face traumatic incidents, moral dilemmas, disrupted sleep cycles, and cumulative occupational stress that rarely manifest in a single domain. Instead, they erode well-being in complex and interconnected ways (Carleton et al., 2018; Stanley et al., 2016).
The MyOmnia model draws upon several foundational frameworks to define and operationalize wholeness. One of the primary influences is the PERMA model of well-being developed by Seligman (2011), which identifies five core elements of human flourishing: Positive Emotion, Engagement, Relationships, Meaning, and Accomplishment. These elements are incorporated into MyOmnia’s domain structure to ensure the model reflects both psychological resilience and life satisfaction.
The MyOmnia approach also reflects the Bio-Psycho-Social-Spiritual model originally proposed by Engel (1977), which emphasizes that well-being is determined not only by biological or psychological factors but also by social context and spiritual meaning. This model remains particularly relevant in the context of trauma-informed care and holistic interventions, both of which are essential in responder populations.
Additionally, the MyOmnia Screener incorporates constructs from the Transtheoretical Model of Change (Prochaska & DiClemente, 1983), which acknowledges that individuals vary in their readiness to engage in behavioral change. By assessing an individual’s stage of change, MyOmnia tailors support recommendations that align with their motivational readiness. This increases the likelihood of engagement and follow-through in wellness interventions (Norcross, Krebs, & Prochaska, 2011).
Finally, the platform integrates principles from prevention science, focusing on the early identification of risk factors and the strengthening of protective factors to mitigate the development of psychological distress (Bradshaw, 2021). The MyOmnia model organizes well-being across seven interconnected domains that span physical, emotional, relational, vocational, and existential dimensions. These are explored in more depth in the assessment design section.
By combining these frameworks, the MyOmnia concept of wholeness reflects a shift from reactive to proactive care. It recognizes that health is not a binary state but a continuum, and that meaningful intervention requires a full understanding of the individual's life context, internal resources, and social environment.
Wholeness, as defined by MyOmnia, is not an idealized endpoint but a practical and measurable state. It reflects the individual’s ability to adapt, engage, recover, and connect across core life domains. This definition supports a proactive model of care, positioning well-being as something to be cultivated, supported, and sustained especially in populations facing chronic and complex occupational stress.
The field of mental health assessment is rich with validated instruments designed to screen for specific psychological symptoms, diagnose disorders, or measure subjective well-being. Tools such as the PHQ-9 (Kroenke, Spitzer, & Williams, 2001), GAD-7 (Spitzer et al., 2006), CESD-R (Eaton et al., 2004), and the State-Trait Anxiety Inventory (Spielberger, 1983) are widely used and scientifically sound. However, while these instruments perform well in clinical diagnosis or single-construct measurement, they fall short in capturing the full complexity of human well-being, particularly in high-stress populations such as first responders.
Most traditional assessments operate within a problem-centric and symptom-focused paradigm, identifying only the presence and severity of pathology. They are designed for use in clinical or research settings, often with the goal of confirming diagnoses. This narrow approach limits their utility in preventive care, where the goal is to detect risk early, support resilience, and enhance functional capacity before a crisis develops. In occupational settings where individuals are unlikely to self-identify or where stigma prevents disclosure, such tools offer limited value (Haugen, Evces, & Weiss, 2012; Corrigan, 2004).
Further, these tools typically treat mental health as an isolated variable, disconnected from vocational stress, social support, spiritual health, or personal purpose. Yet there is robust evidence that mental wellness is shaped by the dynamic interaction of multiple life domains (Keyes, 2002; Engel, 1977). For example, chronic sleep deprivation, moral injury, or financial strain may not produce immediate clinical symptoms but can serve as powerful upstream predictors of future psychological decline (Stanley et al., 2016; Hobfoll et al., 2007).
The MyOmnia Wholeness Screener was created to address a longstanding gap in the field of wellness assessment. Rather than relying on static, one-size-fits-all tools, it introduces a dynamic, person-centered model that adapts in real time to the user’s self-reported needs. Its logic-driven design activates targeted subdomains only when concern is indicated, reducing assessment fatigue and enhancing clinical relevance. This responsive format aligns with leading practices in behavioral health, which emphasize ecological validity and tailoring assessments to reflect the complexity of real-world experience (De Los Reyes & Kazdin, 2005).
One of the most important innovations in the MyOmnia Screener is the Readiness to Change score, which evaluates not just need, but motivation. Derived from the Transtheoretical Model of Change (Prochaska & DiClemente, 1983), this feature allows support to be matched based on the user’s willingness to engage in behavioral change. Research consistently shows that alignment between readiness and intervention increases adherence, reduces dropout, and improves clinical outcomes (Norcross, Krebs, & Prochaska, 2011). Traditional tools offer no such adaptive logic, delivering uniform results regardless of context or motivation.
Another critical differentiator is the Screener’s population-specific design. First responders, healthcare workers, and other high-stress professionals require a tool that reflects the psychological demands of their role. Studies show that trauma exposure, shift work, occupational silence, and moral injury are embedded in these professions and interact with personal health in complex ways (Carleton et al., 2018; Fox et al., 2020). The MyOmnia Screener was built with these realities in mind. Its domains include not only emotional and physical health but also vocational satisfaction, relational quality, spiritual connection, and the presence of purpose, all key factors in sustaining long-term resilience and meaning-making under pressure (Koenig, 2012; Pargament, 1997).
Lastly, the Screener is embedded in a platform that provides data-informed, real-time feedback. Individual users receive immediate, personalized summaries of their strengths and vulnerabilities, while organizations access de-identified, aggregated dashboards showing trends over time. This dual insight model supports a culture of proactive care, allowing organizations to intervene early and build psychologically supportive environments. Traditional tools, by contrast, were never designed for system-level reporting or strategic health planning.
Therefore, the MyOmnia Wholeness Screener is not a replacement for diagnostic screening, it is a complementary and preventive instrument, optimized for environments where complex stress, performance demands, and psychological silence coexist. It expands the lens of assessment from “What is wrong?” to include “What needs support?” and “Is this person ready to act?” This expanded scope is what allows MyOmnia to serve not only as a screening tool, but as a gateway to actionable, individualized, and scalable wellness interventions.
The MyOmnia Wholeness Screener is a clinically informed, multi-dimensional assessment tool designed to measure wellness comprehensively across life domains relevant to sustained health and resilience. Its structure reflects a core tenet of modern mental health science: well-being is not unidimensional, nor is distress reliably captured through symptomology alone. This Screener operationalizes the concept of wholeness through a dynamic, adaptive assessment model that identifies both protective strengths and emerging risks while accounting for personal motivation and readiness to change.
The tool was specifically designed for high-risk, high-stress occupational groups including first responders, whose wellness needs often go undetected or inadequately addressed due to fragmented assessment tools, cultural stigma, and lack of early intervention models (Haugen et al., 2012; Carleton et al., 2018). The MyOmnia Screener bridges these gaps by providing a concise, user-responsive evaluation that adapts in real time based on individual self-report.
The Screener begins with nine high-level items, each corresponding to one of seven foundational domains of wellness. Building on the domains outlined earlier, the Screener uses each to guide the adaptive assessment logic and subdomain triggers. Each item is scored on a 1 to 10 Likert-type scale, allowing the user to self-assess their functioning in that area.
Scores of 7 or lower activate targeted subdomain questions. These subdomains offer deeper insight into the specific factors contributing to diminished wellness in that area. For example, a low score in the Mental domain may activate items assessing depression, anxiety, emotional regulation, functional impairment, and trauma-related stress. Similarly, a low score in the Vocational and Financial domain could trigger items related to work-life conflict, financial strain, or burnout.
This structure reflects contemporary best practices in behavioral health assessment, aligning with guidance from Kazdin (2007) and De Los Reyes and Kazdin (2005) that effective mental health screening must be personalized, ecologically valid, and tied to specific intervention targets. The MyOmnia Screener is not merely diagnostic but directional. It is designed to inform care pathways by identifying not only what is wrong but where and why, while also capturing individual strengths that can be reinforced.
The Screener's design draws directly from decades of empirical work in psychology, occupational health, and public mental health. The following domains were selected based on a comprehensive literature review and field validation (Willoughby, 2024), as well as alignment with theoretical models such as PERMA (Seligman, 2011), the Bio-Psycho-Social-Spiritual model (Engel, 1977), and prevention frameworks in health psychology (Bradshaw, 2021).
Each of these domains includes subdomains and items that were tested in a national validation study, with results demonstrating strong internal reliability and concurrent validity with gold-standard clinical instruments (Willoughby, 2024). Domain intercorrelations further confirm the multidimensional nature of wellness and the value of measuring it through a networked model rather than isolated categories.
In addition to wellness domain scores, the Screener includes two high-leverage assessment items that enhance its clinical utility: the Readiness Score and the Critical Item trigger.
Readiness to Change Score
This item asks the user to rate their willingness to make meaningful changes in the area they identified as a concern. Readiness is a critical predictor of intervention success (DiClemente et al., 1991) and is drawn from the Transtheoretical Model of Change (Prochaska & DiClemente, 1983). Assessing readiness enables practitioners and AI-guided systems to deliver stage-appropriate interventions. Users with high need but low readiness can be matched with motivational enhancement or peer support strategies, while those with high readiness can be offered goal-oriented, skills-based programs. This supports a precision care model that avoids overprescription or misaligned interventions.
Critical Item Detection
This item provides a direct prompt: "Are you currently facing a distressing issue that you would like support for right away?" This open-ended yet targeted question functions as a triage tool for identifying acute risk, including suicidality, substance use crises, domestic violence, or other high-concern scenarios. When a critical item is flagged, MyOmnia’s clinical response team is immediately alerted, ensuring a safety-first protocol without requiring the user to initiate complex reporting procedures. This mechanism is supported by evidence from risk management research, which suggests that direct, well-phrased prompts significantly increase the likelihood of disclosure in high-risk populations (Gould et al., 2005).
Upon completion, each user receives a personalized report detailing their total Wholeness Score (out of 70), their Readiness Score, and color-coded ratings by domain. Domains scoring below 7 are coded yellow or red to flag moderate or high concern. Each domain is paired with brief explanations and recommendations for next steps, which can include access to self-guided content, connection to a peer specialist, or referral to a licensed mental health professional, depending on severity and readiness.
For organizations, de-identified and aggregated Screener data is displayed through a real-time dashboard that enables leadership, wellness coordinators, and clinical teams to identify trends, monitor population risk levels, and deploy resources proactively. These insights are especially valuable in environments like emergency services and healthcare, where teams often underreport distress due to stigma, culture, or time constraints (Fox et al., 2020).
This dual-level functionality, individualized care pathways and population-level visibility, is what positions the MyOmnia Screener as a cornerstone of a modern, preventive mental health infrastructure. It is not a diagnostic tool in the traditional sense, but a structured system for wellness discovery, risk prediction, and engagement enhancement.
The MyOmnia Wholeness Screener uses a structured scoring system that transforms individual self-assessments into actionable insights. The design of this system supports rapid interpretation, personal relevance, and clinical precision. It allows users to understand their wellness profile at a glance while enabling organizational stakeholders to identify trends and allocate resources effectively.
Each of the Screener’s seven core domains is rated on a 1 to 10 scale based on the user’s self-reported perception of well-being in that area. These domain scores are then summed to generate a Total Wholeness Score, ranging from 7 (lowest possible wellness) to 70 (highest). This total score provides a quick overall snapshot of an individual’s wellness and allows for longitudinal tracking over time.
Subdomain scores, which are activated when a core domain score falls below 7, are also recorded on a 1 to 10 scale and averaged across all relevant items. These provide deeper diagnostic precision and highlight the specific drivers of distress or resilience within a domain.
In addition to the wellness domains, the Screener includes a separate Readiness Score that captures an individual’s self-rated motivation to make changes in their area of concern. This score also ranges from 1 to 10 and plays a critical role in tailoring interventions to match the individual’s current stage of change (Prochaska & DiClemente, 1983).
Each domain and the total Wholeness Score are interpreted using a color-coded alert system:
This alert system is grounded in risk stratification theory and aligned with triage-informed mental health models that prioritize early intervention (Belsher et al., 2019).
The MyOmnia platform uses these scores to dynamically tailor content and support recommendations. The system integrates user data into its AI algorithms to generate:
Because scores are tracked longitudinally, the system is capable of identifying not just static wellness states but changes in trajectory, which may indicate improvement, stagnation, or deterioration.
On the organizational side, anonymized and aggregated scores feed into real-time dashboards. These dashboards allow wellness leaders, clinical teams, or command staff to:
This dual-level insight architecture ensures that both individual and organizational needs are addressed, creating a closed feedback loop between assessment, intervention, and evaluation.
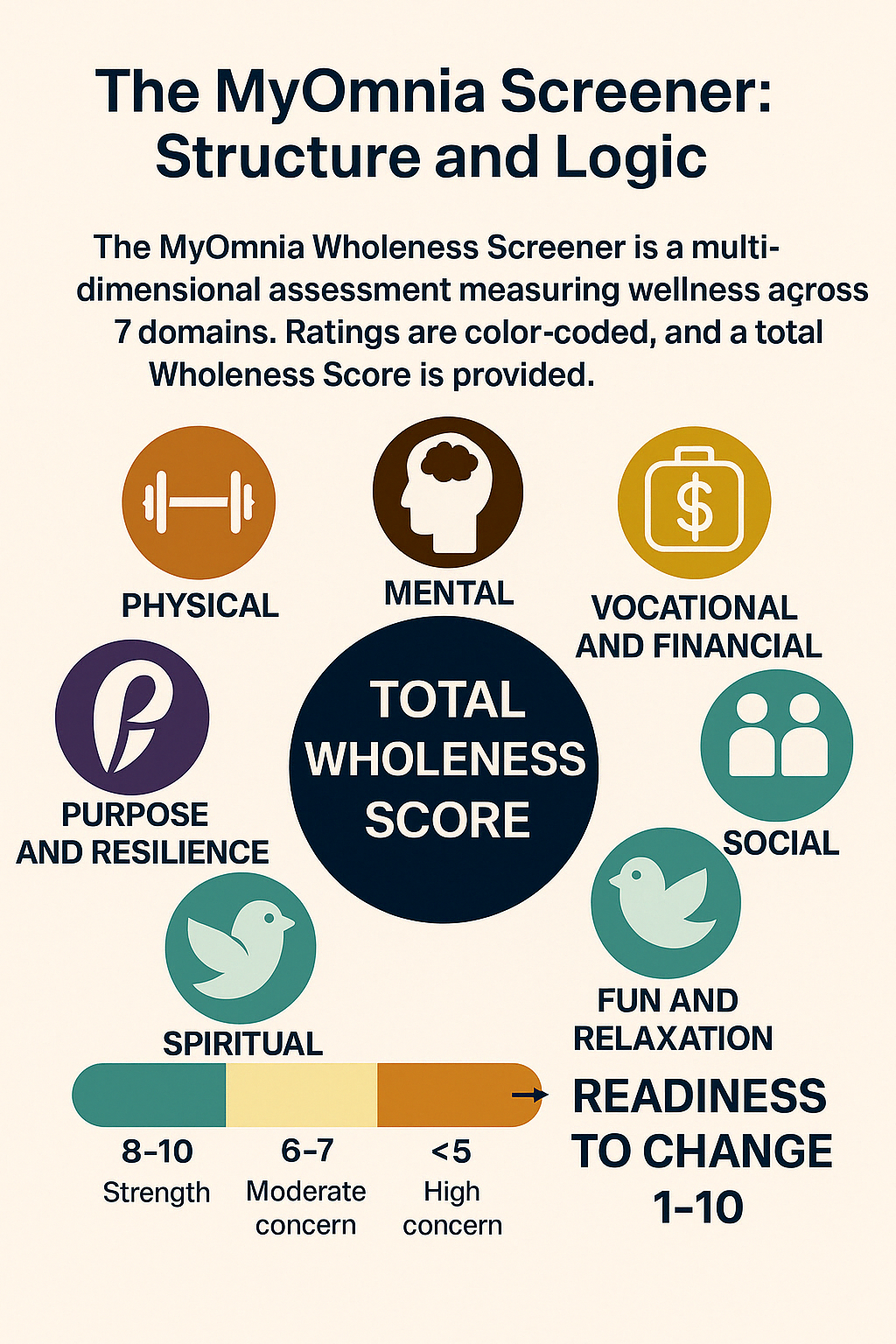
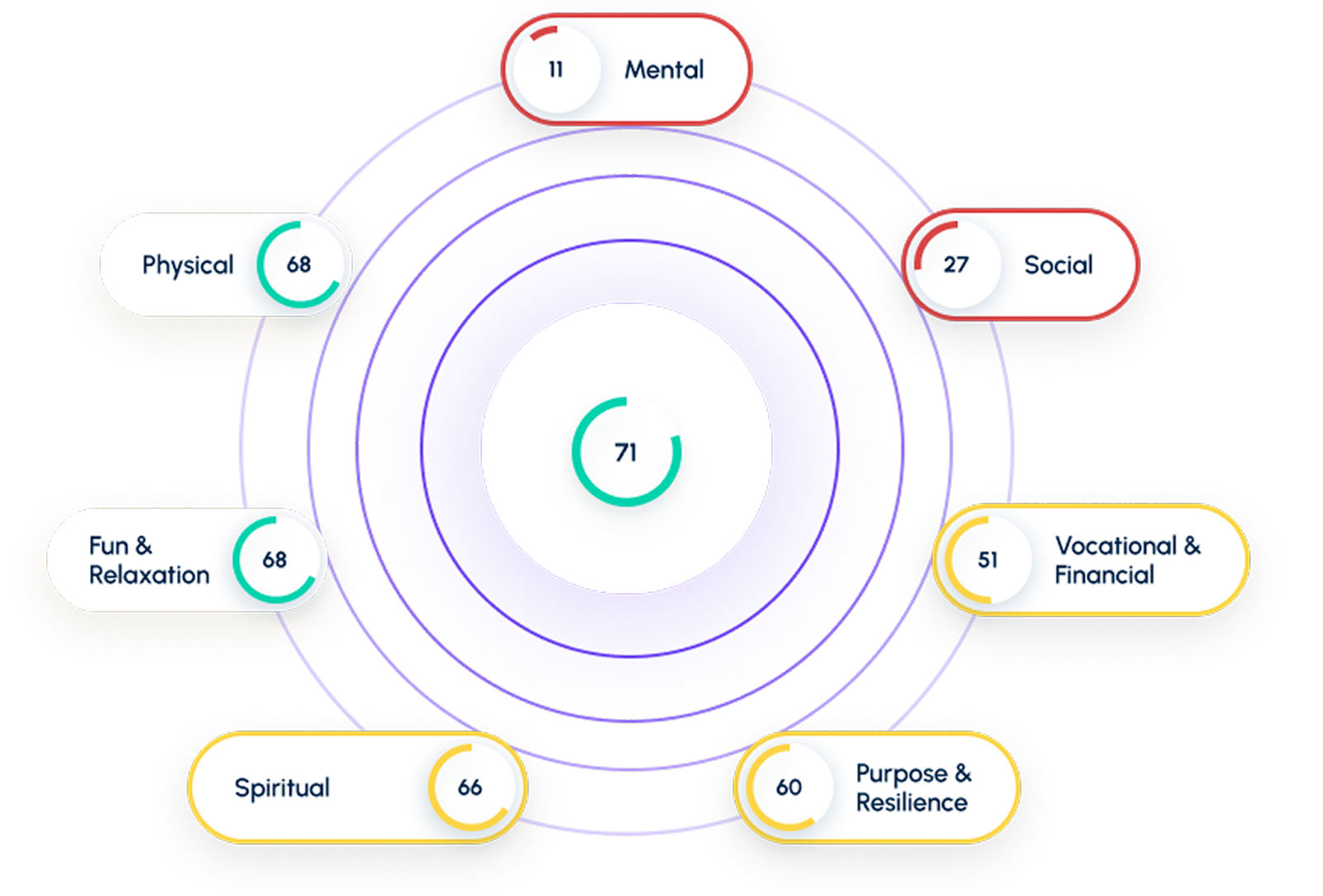
Figure 1: Visual Framework of the MyOmnia Wholeness Screener
This image illustrates the structure of the MyOmnia Wholeness Screener, a multidimensional wellness assessment designed to evaluate well-being across seven domains: Physical, Mental, Vocational and Financial, Social, Fun and Relaxation, Spiritual, and Purpose and Resilience. Each domain is rated on a color-coded 1–10 scale, where:
The screener provides an overall Total Wholeness Score, alongside a Readiness to Change score, which helps guide personalized interventions based on motivation and need. This system supports both individual insight and organizational wellness strategies, particularly for high-stress professions like first responders.
The development of the MyOmnia Wholeness Screener was grounded in a rigorous psychometric validation study conducted by Dr. Brian Willoughby in 2024. The primary objective was to establish the Screener’s reliability, construct validity, and clinical relevance as a tool for assessing multidimensional well-being across diverse populations, with specific attention to high-stress professions such as first response.
The study utilized a national sample of 228 adults residing in the United States, recruited through Prolific, a widely used online research platform. Participants represented a broad range of ages (18 to 73), genders, and ethnic backgrounds. They completed the draft version of the MyOmnia Wholeness Screener along with several established clinical instruments.
The assessment was administered via Qualtrics. Built-in data quality protocols were used, including attention checks, response time monitoring, and duplicate response prevention to ensure data integrity.
The development of the Screener followed a structured, multi-phase process designed to ensure both scientific rigor and practical utility. The initial item pool was generated through an extensive literature review and expert consultation in behavioral health, clinical psychology, and occupational wellness. Constructs were selected based on their empirical relevance to well-being and their utility in high-stress populations such as first responders and healthcare professionals.
Seven core domains formed the foundation of the Screener: Physical, Mental, Social (Relational), Spiritual, Vocational, Fun and Relaxation, and Purpose and Resilience. These domains were conceptually grounded in validated models such as Seligman’s PERMA framework, Engel’s Bio-Psycho-Social-Spiritual model, and principles from prevention science and resilience theory.
Candidate items for each domain were developed and refined through multiple pilot testing rounds. Items were evaluated for clarity, cultural neutrality, and theoretical alignment. Psychometric filtering followed, including analysis of internal consistency (Cronbach’s alpha), skewness and kurtosis for normality, and item-total correlations. Only high-performing items were retained, resulting in three to four items per domain.
The finalized Screener was then tested in the national validation study, with intentional demographic variability to enhance generalizability. The process reflects MyOmnia’s commitment to creating a tool that is both accessible and scientifically credible.
Internal consistency reliability was measured using Cronbach’s alpha. Notable results include:
The reliability analysis confirmed high internal consistency across all major domains, with several exceeding the 0.90 threshold. These metrics are presented in Table 1.
In addition to strong internal reliability, the Screener demonstrated robust construct validity through correlations with validated external measures. Concurrent and convergent validity were assessed using:
These results confirm strong evidence of convergent validity for distress-related domains (e.g., depression and anxiety), as well as divergent validity for protective factors such as resilience, purpose, and social functioning. Notably, the internal Resilience subdomain correlated strongly with the BRS (r = 0.790), and the Attachment domain was strongly inversely correlated with social withdrawal (r = –0.553), confirming the Screener’s ability to detect both vulnerability and strength across life dimensions.
The validation study confirmed that the MyOmnia Wholeness Screener meets key psychometric standards for both individual and organizational use. Its brevity, adaptability, and multidimensional design make it especially suited for high-volume, high-stress environments such as emergency services, healthcare systems, and educational institutions. By synthesizing key psychological constructs into a single, streamlined tool, MyOmnia reduces reliance on multiple fragmented assessments.
The inclusion of the Readiness Score and Critical Item detection adds further clinical value. These features support triage-level differentiation based not just on distress levels but also on motivation and acuity, enabling more personalized and effective intervention strategies.
Operationally, the Screener allows for real-time monitoring, wellness trend tracking, and outcome-based planning. It aligns closely with trauma-informed and prevention-first approaches to mental health, empowering organizations to proactively support their workforce.
In summary, the 2024 validation study led by Willoughby confirms that the MyOmnia Wholeness Screener is a psychometrically reliable, clinically relevant, and operationally scalable solution for evaluating and enhancing well-being in diverse, high-stress populations.
The MyOmnia Wholeness Screener is not merely a tool for assessment, it is a foundational component of a preventive and responsive well-being strategy. By delivering immediate, personalized insights at the individual level and real-time aggregated data at the organizational level, it creates a dual impact that addresses both personal growth and systemic health outcomes.
At the individual level, the Screener facilitates deep self-insight by offering a structured, non-clinical reflection on key areas of life functioning. It allows users to identify areas of strength and vulnerability across domains such as physical health, emotional well-being, purpose, relationships, and vocational satisfaction, many of which are often overlooked in traditional wellness surveys or mental health check-ins.
Building on the readiness-based model described earlier, the platform ensures that support is calibrated not only to need but to personal motivation. This approach increases psychological safety and helps avoid overwhelming individuals with generalized or premature interventions. Instead, it promotes tailored pathways based on both need and willingness to engage, a strategy shown to improve outcomes in mental health and behavioral coaching (Norcross et al., 2011; Miller & Rollnick, 2012).
Personalized feedback following completion of the Screener offers direct, actionable recommendations. These may include evidence-based micro-skills, targeted resilience-building resources, or invitations to engage in peer or professional support. Over time, users can track their progress, revisit domains, and observe measurable shifts in their total Wholeness Score, providing a sense of agency and long-term engagement.
For organizations, the Screener offers real-time visibility into workforce well-being, something traditional surveys often fail to deliver. De-identified, aggregated data provides leaders with insights across units, shifts, or demographics, allowing for early detection of stress patterns, burnout trends, or recovery deficits.
In high-risk professions such as public safety, military, healthcare, and education, this level of insight is critical. Research shows that psychological distress in these environments often goes unreported due to stigma, cultural silence, or time constraints (Haugen et al., 2012; Carleton et al., 2018). The MyOmnia Screener provides a psychologically safe, quick, and accessible way to surface these needs without requiring individuals to self-disclose in a clinical setting.
By integrating Screener insights with existing organizational infrastructure, such as Employee Assistance Programs (EAPs), peer support initiatives, wellness officers, or human resources systems, organizations can implement a tiered support model. High-risk individuals can be referred to licensed professionals, moderate-risk individuals may be matched with guided peer interventions, and those showing readiness can be empowered with proactive resources.
This structure aligns with prevention science and trauma-informed systems, which emphasize the importance of universal screening, early detection, and scalable response models (Bradshaw, 2021; SAMHSA, 2014). Additionally, regular administration of the Screener enables longitudinal tracking, providing organizations with outcome data to assess the effectiveness of wellness programs, training, or cultural interventions.
At scale, the MyOmnia platform contributes to the development of psychologically safe, health-promoting workplace cultures. It normalizes reflection on personal wellness, reduces stigma associated with mental health conversations, and provides leadership with the tools to respond in real time, not reactively after crises occur.
Rather than functioning as a check-the-box initiative, the Screener becomes a core pillar of workforce strategy, helping organizations move from reactive crisis management to proactive well-being leadership.
The development and validation of the MyOmnia Wholeness Screener represent a major advancement in the field of integrated mental wellness assessment. Yet its true potential lies not only in what it has achieved thus far, but in the opportunities it creates for continued innovation, deeper personalization, and broader impact across diverse professional settings.
While the initial focus of the MyOmnia Screener has been on first responders and other high-risk occupational groups, its multidimensional and modular design makes it readily adaptable across a wider range of populations. Emergency medical technicians, dispatchers, military personnel, educators, and correctional officers all face unique occupational hazards that affect mental health, including exposure to trauma, organizational stress, and role-specific moral injury (Papazoglou & Tuttle, 2018; Johnson et al., 2020). Each of these groups may benefit from tailored versions of the Screener that maintain its core structure while adapting language, subdomains, and content pathways to reflect professional context.
Such customization enhances engagement and clinical relevance. Research in occupational health consistently shows that wellness tools are most effective when they are culturally congruent and job-relevant (Quick et al., 2013). The flexibility of the MyOmnia Screener allows it to be embedded in organizational ecosystems without requiring fundamental redesign.
As the volume of usage data grows, MyOmnia will increasingly leverage predictive analytics and machine learning models to anticipate emerging risks, rather than merely responding to reported concerns. This shift from reactive assessment to predictive modeling reflects a larger trend in behavioral healthcare toward precision mental health, the use of real-time data to customize support based on individual trajectories and risk profiles (Insel, 2017).
For example, repeated downward shifts in domains like Purpose or Social Connection, even in the absence of clinical distress, may signal the early onset of burnout or disengagement. Similarly, combining self-reported wellness scores with behavioral engagement patterns (e.g., repeated critical item flags, skipped assessments, or declining readiness) could be used to trigger earlier, more targeted outreach.
By training these models on longitudinal datasets, the MyOmnia platform will be able to proactively recommend content, interventions, or human touch points before traditional symptoms emerge, aligning with the goals of preventive psychiatry and stepped care systems (Bower & Gilbody, 2005; Bradshaw, 2021).
A core limitation of most mental health screeners is that they offer a static snapshot, a single point in time. In contrast, the MyOmnia Screener is built to support ongoing monitoring and change tracking. Individuals can assess their well-being regularly and observe movement across domains, generating longitudinal wellness profiles that can inform personal reflection, clinical conversations, or coaching plans.
For organizations, longitudinal data provide visibility into workforce-level trends and intervention outcomes. This enables wellness leaders to measure the effectiveness of programs, identify seasonal or situational stressors, and build a feedback loop between employee experience and organizational strategy.
Crucially, such tracking supports not only the detection of deterioration but also the celebration of improvement. In high-stress roles where progress is often invisible, showing measurable gains in resilience, social connection, or purpose can contribute to morale, motivation, and retention.
The future of MyOmnia also includes deeper customization by professional role, cultural context, and geographic region. While the foundational domains of wholeness are universally applicable, their expression and perceived importance can vary widely. For example, spiritual well-being may take different forms in a paramilitary culture compared to a hospital environment. Similarly, work-life balance may be experienced differently by night-shift personnel or those in rural dispatch centers.
Future iterations of the Screener will include configurable modules that allow organizations to prioritize certain domains, rephrase context-specific items, and incorporate localized resources. This makes the platform not only scalable but globally adaptable, maintaining psychometric integrity while honoring cultural and contextual nuance.
The MyOmnia Wholeness Screener represents a significant advancement in how mental wellness is understood, measured, and supported, particularly in high-stress professions. Grounded in scientific rigor and clinical sensitivity, it fills a critical gap in the behavioral health landscape by offering a validated, multidimensional tool that not only identifies risk but also elevates resilience, personal strengths, and readiness for change.
While traditional assessments focus narrowly on symptoms, the MyOmnia model offers a broader, more integrated understanding of well-being. It accounts for the interplay between emotional health, physical functioning, vocational satisfaction, relational support, spiritual meaning, and personal purpose, factors long recognized as essential to sustainable mental health but often overlooked in conventional screening approaches. Mental wellness, as MyOmnia reflects, is not a static trait but a dynamic process influenced by life demands, social environments, and individual agency.
By weaving together insights from resilience theory, prevention science, and the Transtheoretical Model of Change, MyOmnia brings a new level of relevance and impact to mental wellness strategies. Its features, including the Readiness Score and Critical Item detection, ensure interventions are both timely and tailored to the user's motivation and urgency. Simultaneously, real-time dashboards offer organizational leaders a proactive lens on workforce wellness, enabling early support and informed decision-making.
In today’s climate of escalating burnout and system strain, especially among mission-driven professionals like first responders, educators, and healthcare providers, the need for a comprehensive, preventive model has never been more urgent. These individuals require more than just symptom tracking, they need systems that are flexible, responsive, and human-centered.
The MyOmnia Wholeness Screener is not just a measurement tool. It is a catalyst for cultural transformation. It empowers individuals to engage with their own mental health, reduces stigma around seeking help, and equips organizations with the insights needed to lead with foresight, compassion, and accountability.
As global awareness of mental health deepens and demands on service professionals continue to rise, MyOmnia offers a forward-looking solution, one rooted in science, built for resilience, and committed to the flourishing of people, teams, and the systems they sustain.
Below are example items drawn from the MyOmnia Wholeness Screener, reflecting the tone, structure, and purpose of the assessment. These are rated on a scale from 1 (very poor) to 10 (excellent) and are designed to encourage reflective, non-pathologizing responses.
If a respondent rates any domain 7 or lower, targeted subdomain items are activated to explore potential drivers of that score.
These results confirm the Screener’s capacity to reliably assess wellness across a broad population and a range of constructs central to psychological functioning.
Asma Nisa holds a Ph.D. in Psychology from the National University of Sciences and Technology (NUST) and serves as a Mental Health Researcher at MyOmnia Wholeness. She is a Clinical Psychologist with extensive experience in psychotherapy, psychological assessment, and transdiagnostic mental health treatments. As the first researcher to implement the Unified Protocol for emotional disorders in Pakistan and a certified Unified Protocol therapist, her work bridges evidence-based science with real-world application. She has contributed to peer-reviewed journals, international conferences, and white papers on emotion regulation, psychological well-being, and psychospiritual approaches to care.
Published on: April 2025